Under Wraps — The Menstrual Narrative
Dr. Liz Lee

When I was at medical school one of my fellow students said to a rather grand surgeon with eight children “Congratulations sir, I hear your wife has had a period”. We thought it was very funny at the time although the consultant apparently didn’t.
Women in the developed world now menstruate many more times than they ever have before. We can expect to have about 400 periods in our lifetime whereas women born in the mid-nineteenth century had about 200. There are several reasons for this. The first is that with better health and nutrition the average age for the onset of menstruation has gradually dropped over the last 150 years from 16 to 13. But more significant are the changes to our patterns of childbearing and breast feeding. Breast feeding inhibits ovulation in most women and so each child born and breast fed for 6 months may prevent about 20 periods. The huge reduction in average family size has thus led to a significant rise in the total number of periods.
As well as the obvious day to day advantages to having fewer periods there are also a number of highly significant medical ones. It has been argued by the contraceptive researchers Couthinho and Segal that the ‘incessant ovulation’ that we now experience is detrimental to our health. Studies show that up to a third of women report heavy periods and slightly more suffer significant pain each month. Premenstrual bloating, breast tenderness, headaches and irritability cause significant morbidity and anaemia as a result of menstruation and is one of the commonest causes of chronic ill health in the world. But perhaps most worrying of all is that an increase in both ovarian and endometrial cancer is linked to ovulation. The more we ovulate the more likely we are to develop one of these malignancies because ovulation causes an increase in cell division in the womb and the ovary.
Few women manage to get through their 400 periods without consulting a doctor at some time. Most problems occur towards the beginning and the end of our fertile years. After the onset of menstruation our ovaries sometimes take a year or two to get into their stride resulting in the erratic ovulation and chaotic periods that are often heavy and painful. Aspirin, paracetamol and neurofen all help the pain, but the only help for the unpredictable bleeding patterns is to put girls on the pill. For many people the pill equals licence to have sex but for me it equals licence not to have horrible periods. If an eleven year old is in trouble with her periods she should not be denied the pill because of this spurious connection.
The pill was developed as a method of family planning and its other uses have always been of secondary importance to the drug companies. It’s introduction a s a contraceptive in the early 1960’s was a major political event. In the hope of getting accepted as a ‘natural method of family planning’ (thus available to the catholic populations of the world) it was formulated in such a way as to give a monthly bleed that mimicked a woman’s normal menstrual cycle. Although the Catholic church was never convinced by this argument the monthly bleed has been retained when in fact there is no medical reason for such long and regular bleeding. OK, so women like to be reassured that they are not pregnant. But give me the choice between a home pregnancy test once a month or a five day bleed and I know which I will choose.
For many years women have been sorting this problem out for themselves. Most pill takers run packets together over the holidays, exams and special celebrations in order to avoid a period. This is fine for three months at a time but there is a sound medical reason to continue to shed the lining of the womb periodically. If this is not done the risk of endometrial cancer rises.
It is getting the balance that is important. Finally the drug companies have realised how debilitating five days of bleeding every month can be and a new pill is in development. Rather than have a seven day break between packets it will have only three days. Bleeding time will be halved without increasing the cancer risk.
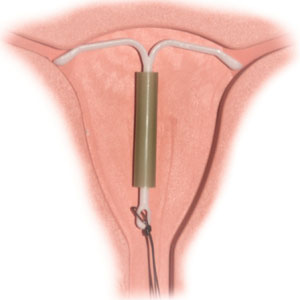
As women approach the menopause their periods often become erratic and heavy as ovulation again becomes sporadic. the most significant recent addition to our vast armoury of medical treatments for these women is not a pill but a coil. The Mirena coil introduced in 1995 is an interuterine contraceptive ‘system’ containing a reservoir of the hormone progesterone which is leaked out in small amounts that are just enough to inhibit the growth of the lining of the womb. Over a period of six months it gradually reduces and then stops the monthly bleed as there is no lining present to be shed. In my own practice the benefits of the Mirena are now becoming apparent as referrals for hysterectomy have dropped by ten percent.
A year ago Sandra Fellows came to see me demanding a referral for a hysterectomy saying ‘I just want it all taken away’. She was pale and exhausted by her frequent heavy periods which confined her to the house for up to three days a month. We talked about the Mirena and she reluctantly agreed to try it on the understanding that I refer her to a gynaecologist if it didn’t work. One year later she is happy with her decision. Although slightly troubled with some irregular bleeding in the first four months she has now completely stopped bleeding. Compared to a hysterectomy with all the attendant risks of major surgery followed by three months convalescence the Mirena is a safe and effective treatment. Provided all goes well she can anticipate very few more periods during her fertile life.
In future years I think those of us who would like to be congratulated for having the occasional period without the trouble of having eight children will be using the pill and the Mirena strategically throughout our fertile lifetimes. We will indeed be more like our great great grandmothers.